By: Dr. W. Scott West, Chief Medical Officer, Nashville Neurocare Therapy
One enduring stigma with mental health is that “it’s all in your head.” This is often stated dismissively, as if you should be able to will yourself to think differently or heal yourself with brute positivity. Understanding mental illness on a physical and chemical level can be validating for those living with mental health disorders.
The truth is, illnesses that are “all in the head” also come back to physical, in-body functions. Your brain is part of your body, after all, just like your arms, eyes, or heart. It is impossible to separate our cognitive functioning from the body, and many mental disorders have chemical and hormonal components. Something being “in your head” doesn’t dismiss its reality in your body and in your lived experience. Your body and mind are inextricably linked, and your mental health deserves the same care, attention, and treatment as any other injury or illness.
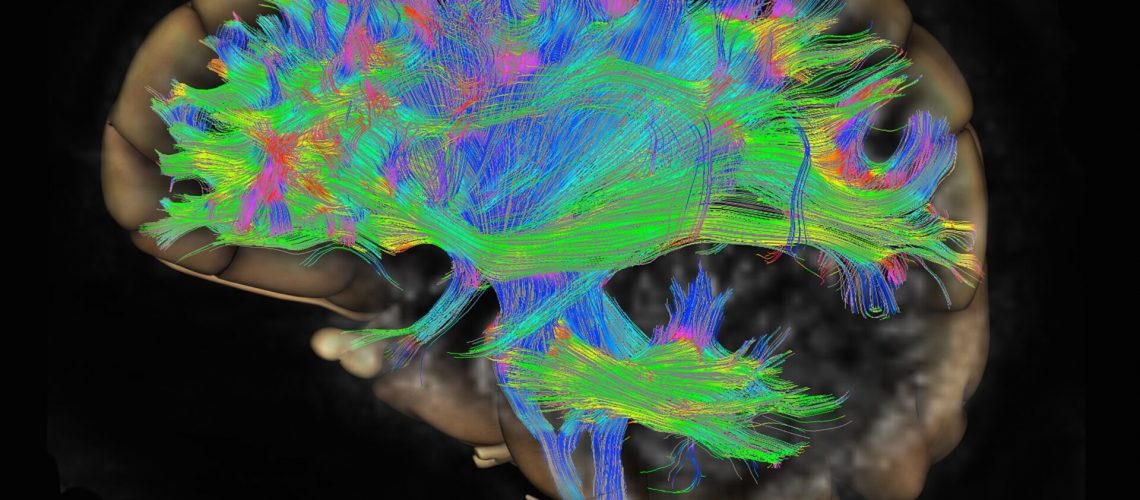
One of the brain functions that influence your mental health is called “connectivity.” Brain circuits connect parts of the brain, and connectivity refers to the strength of these brain circuits. The degree of connectivity between different regions of the brain influences how quickly and accurately these regions can communicate with each other. The quality, fidelity, and speed of that communication impact our feelings and behavior.
Our brains have various circuits for various purposes, like self-reflection, making memories, and detecting threats. Clinical neuropsychology researchers hypothesized that abnormal activity in brain circuits might have something to do with mental illness behaviors. In a 2022 study by Goldstein-Piekarski et al., they used brain imaging technology to observe how “disorders, such as major depressive disorder, obsessive-compulsive disorder, and anxiety, are characterized by altered activity in one or more brain circuits” (Science Connected). The research identified four different brain circuits in particular associated with symptoms of depression and anxiety:
Default mode circuit
Reduced connectivity in the default mode circuit correlates with symptoms of severe negative bias and anhedonia, or the lack of interest in things once found pleasurable. These findings support previous research that found that hypoconnectivity— or reduced connectivity— in the default mode circuit could serve as a biomarker for certain subtypes of depression.
Salience circuit
Individuals diagnosed with anxiety and depression had reduced connectivity in the salience circuit. The hypoconnectivity across this circuit correlates with symptoms like anhedonia, worse life satisfaction, and anxious-avoidant behaviors.
Negative affect circuit
Rather than weak connectivity, the research found that weaker activation in the negative affect circuit correlates with depressive symptoms. In particular, participants diagnosed with depression showed stronger negative bias and faster identification of threatening faces.
Cognitive control circuit
In this study, greater activation in the cognitive control circuit correlated with decreased focus and greater difficulty solving tasks— both of which are well-known symptoms of depression or anxiety.
It’s important to note that not every participant exhibited abnormal connectivity or activation in each of these circuits. All of the behaviors correlated in these circuits are symptoms of depression or anxiety, but different people will experience them to various degrees; for instance, some are more prone to negative affect while others struggle more with cognitive focus.
That being said, this research on the correlation between brain circuit connectivity and activation with the presence of depression and anxiety is preliminary but promising. The hope is that researchers will find an accurate way to use “abnormal circuit activity [to] help determine accurate diagnoses and even predict which types of treatments would work best for each patient” (Science Connected). Equipped with this information, mental health professionals can compare their patient’s brain scans to their symptoms for more accurate and effective identification, diagnosis, and treatment, offering hope for advances in treatment regardless of the uncertainty between the correlation and causation of these symptoms and circuit activity.
While many patients find relief from their depression with talk therapy or antidepressants, many others find their depression resistant to such treatments. TMS Therapy, or transcranial magnetic stimulation therapy, is an innovative therapy that treats depression by stimulating and strengthening the weaker brain circuits that correlate with depressive symptoms. TMS Therapy helps encourage your brain to heal itself by building and strengthening the neural networks that help control your mood and behavior, offering real, lasting relief from depression.
While “stimulating the brain with magnets” might sound a little intimidating, TMS Therapy is not to be confused with electroconvulsive therapy. TMS Therapy is completely medication-free, comfortable, safe, perfectly natural, and has no adverse side effects commonly associated with antidepressants. Though it’s a lesser-known therapy, most private and public health insurances cover TMS Therapy. The American Psychiatric Association lists TMS Therapy as an alternative to antidepressants if your medications aren’t working. If you aren’t finding relief from your depression through talk therapy or medication alone, talk to your doctor about TMS Therapy. Treatment for depression is not one size fits all, and there is hope for you. If you’d like to learn more about TMS Therapy and how it could help you or somebody you love, feel free to request a consultation with our office. We’d love to help you on your journey to healing and wholeness.
About the Author: Dr. W. Scott West
Nationally recognized, board-certified psychiatrist, Dr. W. Scott West, blazed the trail for TMS therapy in Tennessee as the first physician to offer this advanced technology in 2010. With 30+ years experience in clinical depression, Dr. West leads the Nashville Neurocare team.
- Board Certified Psychiatrist
- Specialty: Certified TMS Psychiatrist since 2010
- Diplomate: The American Board of Psychiatry and Neurology
- Distinguished Life Fellow: American Psychiatric Association
- Residency: Vanderbilt University, Hospital Department of Psychiatry
- Medical School: University of Tennessee, Memphis, Center for the Health Sciences
- Hospital Affiliations: St. Thomas Hospital